BPM
- Overview
- Services
- Why Technosoft
- We Can Help
- Showcase
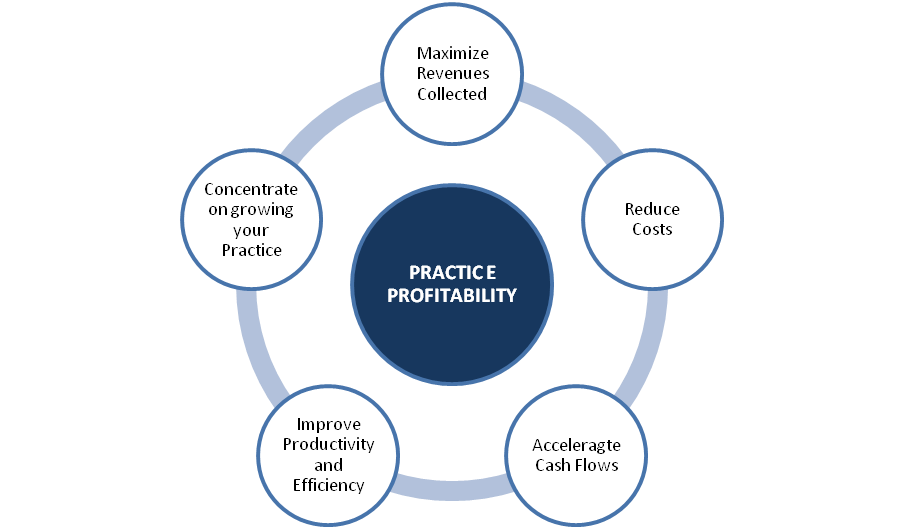
Technosoft offers innovative and comprehensive solutions to medical billing companies and significantly improves their revenue generation capability by streamlining the front and back-end processes through enhanced revenue management capabilities, domain experience, and a robust and customized service delivery platform. Using a state-of-the-art, analytics-driven businesses approach, we help optimize workflows, lower denials and reduce errors in claims processing, thereby increasing revenue, improving efficiency and decreasing operational costs.
We work with some of the largest medical billing companies in the US who rely on our expertise and technology-enhanced solution suite to improve their business processes and performance outcomes, and maximize cost savings.
Our services include:
- Physician Practice Management Services
- Specialty Expertise
- Physician Network Management
- Physician Productivity Improvement
- Revenue Cycle Management Services
- Staffing and Consulting
- Coding and Compliance Services
Benefits
- Expert revenue cycle specialists
- Domain experts in Billing and Coding
- Increased ROI
- Decrease the number of rejected claims
- Improved Cash Flow
- Customer satisfaction
- HIPAA-compliant
- 48 hour turnaround time for Billing and Payment Posting
- Billing Platform-Independent
- Customized MIS reporting
We have partnered with leading companies in the U.S. who rely on our expertise and technology-enhanced solution suite to improve their business processes and performance outcomes, and maximize cost savings.
 |
Medical Billing |

Medical Billing
Medical Billing has become a crucial part of revenue management for healthcare service providers with millions of dollars lost annually due to under-pricing, coding errors, missed charges and un-reimbursed claims due to denials. Technosoft provides turnkey medical billing and coding services to multi-specialty groups and individual physicians in order to reduce costs, increase revenue, improve the accuracy of patient billing, and accurately process bills, while collecting the maximum allowable reimbursement for our clients.
Our services include:
Eligibility Verification
CPT-4 and ICD-9 Coding
ICD-10
Charge/Demographic Entry
Payment Posting
Denial Analysis & Insurance Follow-up
Our experienced billers are familiar with billing practices and methodologies, andmedical terminology and have experience of working on a variety of practice management software such as EPIC, GE Centricity, Imagine, Medical Manager, NextGen, Kareo, Allscripts, Healthpac and more.
 |
Medical Coding |
Medical Coding

Technosoft offers comprehensive coding services as part of our full cycle revenue management and medical billing services, or as a standalone service for organizations doing their own billing. Our analytics-driven approach helps us derive insights by analyzing coding errors to stop rehash denials and our Coding services serve as a core point for generating claim charges, full value reimbursements to providers.
Our solutions are flexible in nature and use innovative technology platforms and automated workflow solutions which offer a variety of reports to track quality and key metrics with value-added services including DNFB reconciliation, Compliance reporting, Provider deficiency reporting and more.
Our Offerings:
Expert coding and Medical record audit services with 95% accuracy
Dedicated team of certified Professional coders
Expert training in coding and documentation
CPT, ICD-9, HCPCS, and DRG coding across various specialties
Clinical Documentation Improvement and Deficiency reporting
Evaluation and management documentation
Chart Auditing
A la carte coding services for all, or a portion, of your requirements
Coding compliance reviews, audits, and monitoring.
ICD 10 migration services
We help leading healthcare companies experience productivity gains and implement higher quality processes, while enabling them to be ICD-10 compliant. Our AHIMA or AAPC credentialed coders providecoding services for leading US hospitals. They have experience in both inpatient and outpatient settings across 25+ specialties and are totally HIPAA complaintand compliant with the Correct Coding Initiatives (CCI) and Local Medical Review Policies (LMRPs). Due to our rapid deployment and set-up, we have the ability to manage a high volume of medical record coding work within a short turnaround time, with an accuracy rate of 95% or more. We are successfully managing the ICD-10 transition for our clients with a full fleet of ICD-10 trainers and credentialed coders.
 |
Revenue Cycle Management |
Revenue Cycle Management

As a leading provider of revenue cycle processing and receivables management services, Technosoft has the depth of experience to improve cash reserves and maximize revenues of Provider organizations (hospital, physician billing company or a physician practice),while streamlining their operations.
Our team of highly-skilled professionals work towards helping your organization’s progress by reducing the cost-to-collect, improving net collections, and using automated technology to derive better process performance, quality, and turnaround time. TWIMS, our proprietary workflow application engine solution automates the receipt, processing and posting of all RCM paper documents, including charges, demographics, insurance payments, patient payments and correspondence.
Key Benefits:
Onsite/Offsite AR subject matter expertise for process consultation
Improved days in AR
AR Analytics with enhanced dashboard reporting
Trained AR callers with an average of 4+ years of healthcare experience
Team with thorough knowledge and understanding of the end-to-end AR process
Experience of working on multiple practice management platforms and multiple specialties.
Continuous learning through training
 |
AR & Denials |
AR & Denials

Technosoft handles all critical functions involved in AR management, including filing of appeals, assessing insurance low pays, updating insurance contracts, managing unapplied balances, managing refunds, and processing patient statements and delinquency letters. We use cutting-edge technology by combining business intelligence and analytics to manage and analyze data, and create information to support business decisions and solve business problems. Our efficient, automated workflow tools provide our clients with extremely detailed and thorough reporting on every claim worked on.
Services include:
A/R Management
Collections
Old A/R,/
Eligibility & Demo Verification
Resolutions focused AR follow-up
Patient Calling and Collections
Denials Management
Credit Balance
Appeals
Correspondence Entry
Root Cause Analysis A/R follow-up
Increased accuracy of claims submission
Lower claim collection time
Reduced claim defaults
Scoring of likelihood of claim approval
Actionable Reporting
Advanced Analytics
Operation and business metrics dashboards
Identification of anomalous trends
Claims denial propensity
Denial trend and root cause analysis
Forecasting tool
Automated eligibility tools
Revenue leakage analysis – Contract coding
Cloud-based solution
Our expertise includes:
Improved Days in A/R(upto38-45 days)
Experienced A/R callers
Enhanced dashboard reporting
AR Analytics and BI Solutions
Better Collections
99% Quality maintained
Periodic Reviews and Training plans
 |
ICD 10 |
ICD 10

With an experienced team of over 1,800+ healthcare professionals, we help our clients mitigate the risk of impending ICD-10 productivity losses, while increasing efficiencies across the enterprise. Underlying analytical solutions help us predict ICD10 revenue loss and help healthcare providers mine existing data for trends and patterns in reimbursement and denials, resulting in high-value, actionable improvements for their Revenue Cycle.
Services include:
Diagnosis Coding
Procedural Coding
Coding Review and Audis
Provider Education & Deficiency Reporting
Clinical Documentation Improvement
RAC Audit
Clinical and Coding Analytics
Coding – Actionable Intelligence
ICD 10 - Gap analysis, Risk and Impact Assessment
Specialty Coding across 15+ Multi-specialties
Dual Coding Support for ICD-9 and ICD-10
Consulting
Auto Audit tools
 |
Analytics |
Analytics

Technosoft helps practices, clinics and physician groups improve their financial status and patient care delivery models by:
Our predictive analytics approach churns the claims data and helps us to confer 95%+ first-pass clean claims rate, while maximizing reimbursements.
Our Offerings:
Monthly Revenue Cycle Dashboards, Variance Root Cause Analysis, Lost Revenue Recovery, Practice Performance Audits, Benchmarking, Payer Contracting Support and System Interface Analysis.
Improve overall patient satisfaction by having the right staff available at the right time.
Improve Patient Outcomes with Accurate Reporting
Our Coding process is structured on automated coding workflow aiming at claim accuracy, efficiency of revenue capturing activities by
Detecting coding errors, while reducing A/R outstanding days, denials and preventing revenue leakage with clinical code recommendations.
 |
Healthcare Information Technology(HIT) |
Healthcare Information Technology (HIT)

Technosoft helps healthcare organizations address complex challenges, including the need to reduce costs, coordinate care, assume more risks and manage complex payment models. Supported by our IT services portfolio, our healthcare IT solutions span across software services and consulting to hospitals, physician offices, imaging centers, home health care agencies and payers.
Technosoft provides Healthcare organizations with the following services;
Application Lifecycle Services
Independent Verification and Validation
Remote Infrastructure Management
Data Sciences
Mobility
Our functional areas of support include
Healthcare Analytics
Provider database automation
Healthcare insurance exchange
Wellness automation
Membership management
Claims management
Un-insured application integration
Social security office support
Technosoft has significant experience in servicing several State and Local Governments including California, Connecticut, Illinois, Kentucky, Michigan, Minnesota, Montana, New Mexico, Pennsylvania, Rhode Island, Washington and Texas. Our collective experience in handling various government functions includes Child Support, Unemployment Insurance, Medicaid, and Eligibility. .
Technosoft specializes in developing and implementing scalable, extensible and configurable solutions across various technology platforms.
ADM (J2EE, .NET, Sharepoint)
Application exposure: Mainframe, MMIS, MITA , Facets , Pega workflow
Data Warehousing and Business Intelligence (TIES)
Independent Verification and Validation
Mobility (MobXL)
Remote Infrastructure Management (TRIMS)
Enterprise Architecture Upgrade Planning Implementation
COTS Implementation & Customization
Transfer Systems Implementation
Software As A Service (SAAS)
 |
Mobility |
Mobility

Being leaders in mobility solutions, with strong offerings, integrated workflows and simple user interface, we help healthcare providers optimize and streamline the way data is entered, accessed, and shared, resulting in improved delivery of care.
Our compelling value proposition, in-depth healthcare domain knowledge, operational capabilities combined with quality will significantly improve the performance and profitability of your business. As a leading Business Process Management services provider and solutions partner, Technosoft is exclusively committed to serving the needs of the US healthcare industry. Technosoft empowers hospitals, physicians and other healthcare organizations to integrate key areas of financial performance and improve their cash flow.
Our solutions are analytics-driven, technology-enabled and backed by appropriate technology platforms, human resource skills and other differentiators such as:
- Integrated Revenue Cycle solution
- Deep multi-specialty expertise – experience handling over 25+ specialties and adaptability to different PMS
- Over 1800+ healthcare specialists across 3 offices in US and India
- Certified resources with AAPC, AHIMA & AAHAM credentials
- ISO 9001 certified since 1999, and HIPAA-compliant
- Graduate workforce with Life sciences, Finance, Biology backgrounds
- Reduced administrative cost by 30% – 40%
- Analytics-driven Self-Pay and Collection Solutions - Better Collections, Fewer A/R days
- Actionable Intelligence with RCM, Clinical and Operational dashboards
- Accelerated cash flow with efficient work flow systems
- Proprietary knowledge management and workflow tools with value-added services such as Provider education and Deficiency reporting
- On-Demand / Scalable Staffing
- Structured, systematic and sustainable transition with quicker ramp-up plans
Technosoft is committed to offering value-added Healthcare BPM + IT solutions to our clients for performance optimization and profitability. We have always aimed to be value partners to our clients, taking pride in their business growth.
We believe true value is best created when our solutions focus on specific client issues and are developed with intensive analysis and expertise. Our diverse offerings are designed to mitigate customer pain points, and also provide comprehensive, sustainable, scalable solutions. We have a large pool of skilled resources, from which we can deploy people in no time to kick-start new engagements, both at our onsite and offshore centers.
Key benefits:
- Significant cost reduction
- 'Best in class' Delivery model
- ICD-10 Solution
- Reduced revenue cycle time and optimize collection
- Structured and organized operations
- Accelerated cash flow
The brighter picture: RCM services boost revenues of Radiology practices
A leading national billing company that specializes in Radiology seeks our ‘Revenue cycle management services’ to boost revenues of their partnering Radiology practices.
Our client assists Radiology practices and health systems to handle their growth and capture every penny by offering detailed and customized solutions for billing, collections, insurance claims processing, staffing, revenue trends, and easing the pressure on reimbursements. As a partner to our client, Technosoft provides customized revenue cycle services with insightful advice and data-driven analysis which helps them boost their associated radiology practices’ revenue goals, and increase collection rates.
Leading billing provider drives up revenue for Emergency / ambulance services companies Leading Medical billing provider increases revenue for Emergency / Ambulance services companies by 20 percent while freeing up 50 percent of time spent on operations.
Technosoft understands that balancing EMS and ambulatory services with business and cash flow needs can be a difficult task. To help EMS systems succeed given the intricacies and demands of our industry, we provide a simplified EMS billing alternative with proven cost effectiveness, streamlined efficiency and unparalleled customer service. Technosoft continually utilizes the latest billing industry methods and best practices—as well as proprietary processes—to help our client maximize its revenues and the efficiency of its business servicing emergency services companies.
Billing & collections services help CHCs manage revenue goals, increase reimbursement rates Community Health Centers /FQHCs utilize Technosoft’s cutting-edge billing and collections services to manage their revenue goals and increase their reimbursement rates.
With burgeoning healthcare costs, federally qualified health center (FQHCs) are struggling to handle their revenue sources, are unsure about whether their commercial contract rates are appropriate and if the terms are fair. There was not enough Data on collections. The Community centers were reeling under low collection rates and higher denial rates with poor revenue cycle services. After experiencing success following our engagement, the client instituted processes to improve the revenue standards of FQHCs, with a focus on previous billing and collections efforts. The FQHCs have collected hundreds of thousands of dollars from previously unpaid claims and substantially reduced their average A/R days
